Every year I am astounded that my skin cancer patients keep getting younger and younger... And I’m not talking about those patients in their 40s and 50s, I’m talking about patients in their 20s and 30s. Yes, we are all at risk for skin cancer. Whether it be due to a genetic predisposition or excessive exposure to the sun‘s harmful ultraviolet radiation, skin cancer can happen to anyone.
As the incidence of melanoma and nonmelanoma skin cancers continue to rise, I am reminded of the importance of patient education, raising public awareness of what to look for on self-screening exams, increasing the accessibility of sunscreens and making sure all people know that it is important for everyone to see a dermatologist regardless of their personal or family history.
I find that while patients might realize their sensitivity to sunlight may be extreme or even moderate even in their youth, understanding that tanning is actually a form of injury to the skin, which can set up fertile soil for skin cancer growth is not something that resonates. That's why I want to raise awareness though this blog, especially during the month of May, so that my friends, family, patients and even complete strangers might understand that taking care of their skin now can prevent serious sun-related injury and deadly skin cancers.
It is empowering as a Mohs micrographic surgeon, to realize that skin cancer is both a very treatable and a very preventable disease. While many cancers grow very slowly, certain cancers including aggressive squamous cell carcinomas and melanoma, can grow quickly and require diagnostic and surgical intervention as soon as possible. While I see nonmelanoma skin cancer in young patients, it is important to realize that the most deadly skin cancer, melanoma, has a higher rate of occurrence in younger patients. Melanoma represents the highest skin cancer-related mortality in patients in their 20s and 30s.
In this first segment, I am going to focus on melanoma, a deadly form of skin cancer that can occur in anyone, any race, any part of the body....even in the eyes. Melanocytes, or pigment-producing cells of the body, when exposed to harmful UV rays, can be damaged through photo-injury which can cause melanoma growth. Melanomas grow first in an early radial growth phase, during which diagnosis is crucial. When melanomas are excised through surgical excision, margins must be large to ensure complete eradication of all atypical cells. The later (vertical) growth phase can often times be too late: this is when roots grow more deeply and distant spread to other organ systems can occur. Surgery is still the mainstay of melanoma treatment but other adjuvant therapies may be required in advanced cases.
[1]
In my practice, I am seeing more and more melanoma in younger patients. It is frightening to think that these aggressive cancers can develop rapidly in healthy, young, vibrant people, but it happens! So read this blog to find out how to keep yourself safe and cancer-free!
What is melanoma and what is the incidence of melanoma?
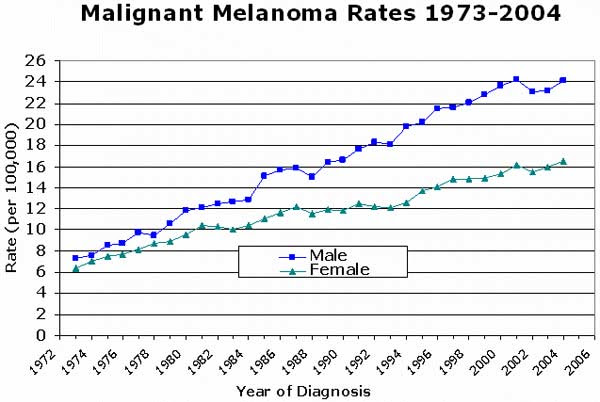
Melanoma is the most serious form of skin cancer and is characterized by the uncontrolled growth of the pigment-producing cells of the skin. Melanomas can grow primarily but also can develop within an existing mole. The overall incidence of melanoma continues to rise and, surprisingly, melanoma rates in the United States doubled from 1982 to 2011. Age-specific indices of melanoma case seem to be growing drastically as well. Male sex seems to impart an increased risk: interestingly rates of melanoma diagnoses in men are rising sharply. [2]


Is melanoma a serious disease?
YES!!! Although completely treatable when detected early, advanced melanoma can spread to the lymph nodes and internal organs, which can be fatal. Approximately 9,320 people will die from melanoma in 2018. [2]
What causes melanoma?
Risk factors for developing melanoma includes the following:
- Ultraviolet light exposure from the sun is linked to 95% of melanoma cases [2]
- Tanning Bed use/exposure; especially in women < 45 [2]
- Living close to the equator. [2]
- Age > 65 - suggestive of cumulative effect of harmful UV rays. [2]
- A history of 5 or more blistering sunburns between ages 15 and 20 increases one's melanoma risk by 80 percent. [2]
- Lighter skin tones and Caucasian race [2]
- history more than 50 moles, unusual moles or large moles on the skin. [2]
- family history of melanoma or personal history of nonmelanoma skin cancer, including squamous cell carcinoma or basal cell carcinoma [2]
- Physical characteristics: history of sun sensitivity, red/blond hair, blue or green eyes [2]
[3]
Does Melanoma have a precancer lesion?
The answer is Yes! Atypical moles are the precursor lesion to a melanoma, although some melanomas arise primarily as full-blown cancer. Suspicious signs of an atypical moles would be larger size, color variability and border irregularity. Some patients have 100s of atypical moles, making them at increased risk for melanoma. [2]
What does melanoma look like?
Use the following ABCDEs of melanoma as a guide for recognizing pigmented lesions that are atypical and require biopsy in some instances.
- Asymmetry: if one half does not match the other half. [2]
- Border irregularity: If the edges are jagged, notched or blurred. [2]
- Color: A lack of uniformity of color, color variability or color variegation. If different shades of tan, brown or black are often present. If spots of red, white, and blue are present, this also suggests atypia. [2]
- Diameter: Larger lesions, greater than 6mm are at increased risk for Melanoma, but melanomas can also be quite small (<1 mm) [2]
- Evolving: if a mole looks different than the rest or demonstrates change over time, including color change, growth, border change. [2]
So stay safe everybody! Here are some tips to protect yourself:
- Everyone needs a skin exam. If you have a mole, a new growth, or one that is changing, it is essential to get this diagnosed and evaluated by a trained professional. Dermatologists need to be the ones that evaluate these suspicious lesions, not general doctors. Dermatologists are specialists that are trained to diagnose and treat skin cancers, precancers and other skin lesions correctly.
- People with a family history of skin cancer, especially melanoma, are at higher risk for melanoma and therefore definitely need routine skin exams yearly.
- People who do not have a family history of skin cancer are still at risk for skin cancers. These physical characteristics are high predictors of increased susceptibility: red or blonde hair, blue eyes, freckling, or lighter skin tones.
- Tanning = solar damage. Tanning is a physical indication that you are not putting on enough sunscreen and/or getting too much sun. While less damaging than a sunburn, tanning represents increased dispersion of melanin with in the epidermal cells called keratinocytes. This is an indication of damage to DNA that is occurring within your epidermal cells. So take tanning as a warning sign: apply more sunscreen, apply more frequently, use better sunscreens and avoid sun exposure.
- Tanning beds are the enemy. These dermatologic nemeses are basically superdoses of concentrated ultraviolet radiation. You are basically frying your skin when you go to the tanning bed. A history of tanning bed use is strongly associated with early-onset melanoma. So PLEASE avoid the tanning beds at all cost!
- If you notice a new mole, a mole different from others on your skin, or one that changes, itches or bleeds, even if it is smaller than 6mm, you should make an appointment to see a board-certified dermatologist as soon as possible
References:
1. American Association of Cancer Research. Clinical Cancer Research. Well-Defined Melanoma Antigens as Progression Markers for Melanoma: Insights into Differential Expression and Host Response Based on Stage; Fig. F. Stephen Hodi; DOI: 10.1158/1078-0432.CCR-05-2616. Published February 2006. http://clincancerres.aacrjournals.org/content/12/3/673.figures-only
2. American Academy of Dermatology. Melanoma; 2018. https://www.aad.org/media/stats/conditions
3. MedIndia. Melanoma. Melanoma; What are the Risk Factors for Melanoma? Published on Jul 25, 2011. https://www.medindia.net/patients/patientinfo/melanoma.htm
4. Mayo Foundation for Medical Education and Research. Melanoma; Overview. https://www.mayoclinic.org/diseases-conditions/melanoma/symptoms-causes/syc-20374884

![[1]](https://images.squarespace-cdn.com/content/v1/5a9c8fd5506fbeffea5abf9b/1526666495544-UZOBFXNV3YL9QY71G0YC/unnamed.jpg)
![[3]](https://images.squarespace-cdn.com/content/v1/5a9c8fd5506fbeffea5abf9b/1526668165070-X23BNYQYO5BW6VSMWUSW/unnamed-4.jpg)


