The Truth about Men and Sunscreen
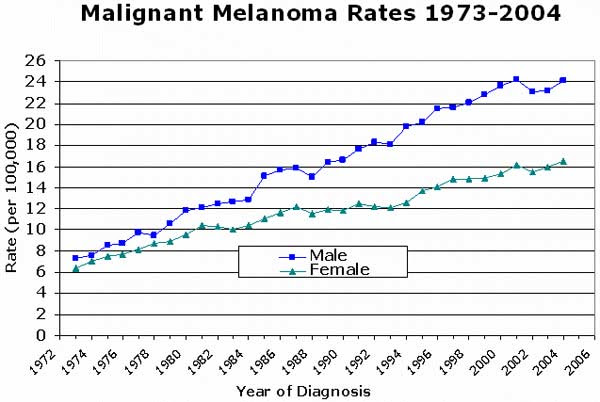
Although the American Academy of Dermatology continues to launch costly prevention campaigns and has boosted public awareness for decades, an important question is posed: why does the incidence of skin cancers continue to soar? However, in this article, I want to focus on skin cancer trends in men.
Here are some alarming statistics: Caucasian men represent the demographic with the highest rate of annual UV exposure and highest rate of melanoma-specific deaths. The annual rate of new melanoma cases in men has nearly tripled in the past 30 years.
So, how could this be? We are living in a world where skin care lines routinely incorporate sunscreen preparations that are both elegant and affordable. Suncreen is seemingly ubiquitous in drug stores and supermarkets. The Skin Cancer Foundation and American Academy of Dermatology fuels millions of dollars into media- and web-based campaigns to educate the public at large. So why does the prevalence of skin cancers continue to soar? Are these prevention campaigns working?
As a Mohs micrographic surgeon and skin cancer specialist, I consistently advocate regular sunscreen use and monthly self-checks to all of my patients, but especially in patients with a higher than average risk. Skin cancers in male patients demonstrate a more aggressive clinical course and are more likely to be fatal, when compared to women. Moreover, in a recent survey, only 51% of male patients reported sunscreen use, and 70% did not know the warning signs of skin cancers. This underscores that just being a man is a risk factor for skin cancer.
As a man, I realize my own weaknesses and limitations. The details and application recommendations for sunscreen use are voluminous and cumbersome to say the least. After reading the guidelines on the American Academy of Dermatology website, I was literally exhausted. Most men would read these guidelines and think, “When am I going to have time to play tennis ?” or “I came here to fish, not to apply sunscreen all day!”
It is true that most patients, especially men, are not thinking about skin cancer while enjoying their family vacation on the beach. However, we really should be. In my opinion this is central to the essence of the problem. We should be thinking about the fact that melanoma is much more deadly in our demographic, compared to women. We should be thinking that skin cancer and premature aging of the skin are entirely preventable. And most important, we should take ownership of our health. And while dermatologists are not asking patients to give up what they love—golfing, boating, surfing, sporting, fishing and fun on the beach—we are asking our patients to be responsible.
So here are some simple guidelines for men, so that we can continue to do the things that we love in the sun, while demonstrating responsibility and honoring our bodies.
Rule # 1: You only get one life and one body, so protect yourself! Use sunscreen! Which sunscreen? Broad-spectrum, SPF > 30, and water resistant. My favorites are Germain Dermatology Super Sheer Spray and Blue Lizard for outdoor activities, since they offer the highest water resistance. SPF 30 blocks 97% of harmful UVB rays. Higher SPFs block only slightly more of the sun’s UV radiation. Broad spectrum refers to sunscreens that offer both UVA and UVB protection. UVA and UVB both cause cancer; however, UVA is responsible for premature aging of the skin.
Additionally, I recommend our sunscreens formulated by Dr. Marguerite Germain. The reason I recommend them so highly is that our patients LOVE them and use them regularly. Why? Because they are non-greasy, totally concealable, and contain naturally-occuring hypoallergenic and superpotent antioxidant ingredients, including green tea polyphenols, CoQ10 and resveratrol, which nourish your skin and provide additional anti-cancer activity. Over-the-counter sunscreens available at your local drug stores and markets may offer broad-spectrum photoprotection but contain toxic preservatives that can be damaging to your body. In my experience, the best way to promote routine skin care among my male patients is to deliver excellent products that make your skin feel and look its best.
Check out our top-of-the-line sunscreens at Germain Dermatology designed for our male patients:
Super Sheer: This ultra-sheer and non-greasy formulation contains 13.75% micronized zinc oxide, along with superpotent concentrations of green tea polyphenols and CoQ10 to provide the ultimate broad-spectrum and antioxidant protection in a cosmetically elegant preparation.
Super Sheer Spray (NEW): This is my favorite! I think it is perfect for male patients, because it is so easy to use for full-body applications on beach days. Super sheer spray also contains superpotent zinc oxide for broad-spectrum sun protection in addition to high concentrations of antioxidants.
Blue Lizard: My favorite for long days on the beach. Blue Lizard offers great broad-spectrum coverage with the highest water resistance available. It is certified by Australian standards, which are manufactured at higher standards than American sunscreens.
Heliocare: An oral dietary supplement with antioxidant effects that promote the skin’s ability to protect itself against sun-related free radical damage.
Rule # 2: How often to apply: Every two hours. I recommend using a buddy system if on the beach with friends. Share the responsibility and remind each other to reapply. Check your friends for red streaks and encourage more frequent application, should you see evidence of burning.
Rule # 3: Avoid sun exposure between the hours of 10 am and 2 pm, during which time UV exposure is most intense.
Rule # 4: ABSOLUTELY NO TANNING BEDS. Use fake tanners or bronzing agents instead! Everytime you think it might look great to have a tan, remember that by virtue of your being a man, you run a greater risk of developing skin cancer. MELANOMA IS DEADLY.
Rule # 5: You feel your best, when you look your best. Protecting your skin from the sun will prevent photoaging (premature wrinkling of the skin), allowing you to look and feel your best! Here are products that are very popular among our male patients:
Magic Eyes: My personal favorite! It is so perfect for men, because we tend to develop deep wrinkles around our eyes over the years. Magic eyes is an elegant eye cream that contains high doses of Vitamin C and green tea polyphenols to prevent and reverse sun-induced wrinkling and aging of the skin.
Retinol Rejuvenation pads: Retinol is an advanced Vitamin A derivative that comes in several formulations that nourish your skin, improve skin tone and reduce fine lines and wrinkles. By increasing cell turnover, retinol also fights against harmful skin cancers! I recommend this highly for patients with a personal history of skin cancer.
Antioxidant cream: an elegant blend of our most bioactive antioxidants prepared in a hydrating serum. It is bioengineered to enhance skin texture and elasticity.
Advanced Vitamin C Serum: This is another favorite! Much more than pure Vitamin C, it is our most concentrated blend of antioxidants, containing L-ascorbic acid, Vitamins A and E, emblica and ubiquinone. This serum is lightweight, hydrating and full of goodness! A perfect fit for our male patients!
Rule # 6: Know the skin you’re in. YOU ARE RESPONSIBLE for your own health. Own this. Do monthly self skin-checks and alert your dermatologist if you notice any new or changing dark spots or red spots. Use the mnemonic ABCDE to identify suspicious lesions. Alert your skin cancer provider should you find dark spots with any of the following:
A: Asymmetry
B. Border irregularity
C. Color variegation
D. Diameter > 6 mm (roughly the head of a pencil eraser)
E. Elevation
Rule #7: Get skin exams yearly with your dermatologist. If you have a history or family history of skin cancer, you need skin exams twice yearly.
Dr. Joe’s tips for supreme #sunsafety:
1️⃣ wear sunscreen everyday and reapply every hour
2️⃣ avoid peak UV exposure from 11 am to 4 pm
3️⃣ wear a sunscreen (spf 30 or higher) that contains a physical blocker like Zinc and protects against UVA and UVB
4️⃣ take heliocare
5️⃣ wear a UV protective broad-brimmed hat and UV protective clothing
6️⃣ if you have a new or changing skin lesion, one that bleeds, or is painful, please see a board-certified dermatologist ASAP for biopsy! Don’t wait until it’s too late !!
7️⃣ if you have a personal or family history of skin cancer, Head to toe skin exams are needed every six months! If you have a personal history of melanoma, skin exams every 3 months x 2 years; then q6 months.
It’s ok to have fun in the sun! Just do it safely! #sunsafety #drjoe
Dr Joe getting his #sunsafety on!














![[1]](https://images.squarespace-cdn.com/content/v1/5a9c8fd5506fbeffea5abf9b/1526666495544-UZOBFXNV3YL9QY71G0YC/unnamed.jpg)


![[3]](https://images.squarespace-cdn.com/content/v1/5a9c8fd5506fbeffea5abf9b/1526668165070-X23BNYQYO5BW6VSMWUSW/unnamed-4.jpg)


